We are deeply grateful for the compassionate care provided by the dedicated staff at our partnering nursing homes. Your commitment to residents is invaluable, and we are honored to work alongside you to enhance their quality of life.
Research shows that strong collaboration between hospice providers and nursing homes leads to improved patient outcomes, higher family satisfaction, and better quality metrics. Here are some key statistics that highlight the impact of our partnership:

Your role in patient care is vital. Every day, you provide comfort, dignity, and support to residents and their families. As we celebrate National Nursing Home Week, we want to recognize your unwavering dedication and the compassionate care you provide.
We are always looking for ways to enhance our collaboration and better serve your residents. If there is anything we can do to support your team – whether through additional training, in-service education, or improving care coordination – please reach out.
Lets continue making a meaningful impact together. Call us anytime.
Thank you for all that you do to support your residents! We are honored to be your partner in care. Happy National Nursing Home Week!
References
Gozalo, P., Teno, J. M., Mitchell, S. L., Skinner, J., Bynum, J., Tyler, D., & Mor, V. (2018). Hospice effect
on government expenditures among nursing home residents. Health Services Research, 53(5), 3437-
3460.
Medicare Payment Advisory Commission. (2019). Hospice services in Medicare: Report to Congress.
MedPAC. https://www.medpac.gov
Miller, S. C., Lima, J. C., & Intrator, O. (2020). Quality of hospice care in nursing homes: Family
perspectives. Journal of Palliative Medicine, 23(7), 900-907.
Teno, J. M., Gozalo, P., Trivedi, A. N., Mitchell, S. L., Bunker, J., Lima, J., & Mor, V. (2018). Site of death,
place of care, and health care transitions among U.S. Medicare beneficiaries, 2000-2015. JAMA,
320(3), 264-271.
During National Hospital Week, we extend our deepest gratitude to the dedicated doctors, nurses, case managers, and healthcare professionals who go above and beyond every day. Your tireless efforts provide healing, comfort, and hope to those in need – especially when life’s journey requires the highest level of care. As a hospice provider, we see firsthand the impact you make on patients and families. Your commitment to excellence and compassionate service allows us to work hand in hand, ensuring that every patient receives the dignity, comfort, and specialized care they deserve at every stage of their journey.
Thank you for your partnership, your expertise, and your dedication to our shared mission of caring for those who need it most.
Let’s continue working together to provide exceptional care – because every moment matters.
Military families understand the meaning of sacrifice—both in service to the country and in caring for
their loved ones. Military caregivers embody selflessness, often providing unwavering support to aging or
terminally ill family members. As a hospice provider, we recognize the distinct challenges these caregivers
face and are dedicated to providing compassionate, specialized care that honors their journey.
The journey of a military caregiver is often shaped by resilience, routine relocations, and the profound
impact of service-related injuries or illnesses. Many veterans may face conditions linked to their service,
such as chronic pain, post-traumatic stress disorder (PTSD), Agent Orange-related illnesses, and
service-connected disabilities. These factors require a hospice provider who is deeply attuned to the
complexities of military caregiving and the unique emotional, medical, and logistical needs of these
families.

Military caregivers face higher rates of stress, depression, and financial strain compared to civilian caregivers (Ramchand et al., 2014). According to the RAND Corporation, military caregivers provide an average of 10+ additional hours of care per week compared to non-military caregivers, often navigating complex health conditions related to service (Ramchand et al., 2014). Furthermore, up to 30% of post-9/11 military caregivers experience clinically significant mental health challenges while supporting their loved ones (Tanielian et al., 2018). Our hospice services alleviate this burden by offering comprehensive, holistic support to both the patient and caregiver.
Medical professionals play a crucial role in guiding military families toward the specialized hospice care they deserve. If you are a provider caring for a veteran or military family, consider referring them to our hospice services to ensure:
If you are a medical provider, we invite you to refer military caregivers and their loved ones to our hospice program. If you are a military caregiver, we are here to walk this journey with you. Call us today to learn how we can support you and your loved one.
We salute your service and honor your sacrifice—both in uniform and in caregiving.
References
Ramchand, R., Tanielian, T., Fisher, M. P., Vaughan, C. A., Trail, T. E., Epley, C., & Robbins, M. W. (2014). Hidden heroes: America’s military caregivers. RAND Corporation. https://www.rand.org/pubs/research_reports/RR499.html
Tanielian, T., Ramchand, R., Fisher, M. P., Sims, C. S., Harris, R., & Harrell, M. C. (2018). Military Caregivers: Cornerstones of Support for Our Nation’s Wounded, Ill, and Injured Veterans. RAND Corporation. https://www.rand.org/pubs/research_briefs/RB9937.html
Every April, we take time to recognize Patient Experience Week, a vital healthcare observance that highlights the commitment of providers, caregivers, and referral partners in delivering compassionate, high-quality care. For those of us in hospice care, this week is a special opportunity to express gratitude for the invaluable collaboration of medical professions like you – who trust us to provide comfort, dignity, and peace to patients during life’s most vulnerable moments.
When a patient is facing a terminal illness, their journey should be met with the highest level of comfort, respect, and support. The decision to refer a patient to hospice is never easy, but together, we ensure that their transition is seamless, compassionate, and focused on quality of life. By working closely with physicians, hospital discharge planners, skilled nursing facilities, and other healthcare partners, we:

Research consistently shows that patients who receive hospice care earlier in their disease trajectory experience higher quality of life, improved symptom control, and better family satisfaction (Teno et al., 2016). Studies also highlight that coordinated transitions to hospice can significantly reduce unwanted hospitalizations and aggressive treatments at the end-of-life, allowing patients to spend their final days in the place they prefer – whether at home, in a hospice residence, or a long-term care facility (Dixon et al., 2015).
Moreover, patient-centered communication and collaboration between referring providers and hospice teams lead to a 70% improvement in satisfaction among families and caregivers (Connor et al., 2020). This statistic underscores the critical role of partnerships in hospice care – ensuring every patient’s experience is defined by comfort, dignity, and peace.
Your dedication to patient-centered care does not go unnoticed. By partnering with our hospice team, you ensure that patients and families receive the respect, comfort, and guidance they deserve in life’s most precious moments. Your referrals make a profound difference – not only in the quality of care provided but in the lasting impact on the families left behind.
This Patient Experience Week, we celebrate you. Thank you for entrusting us with your patients and for your unwavering commitment to their well-being.
If you’d like to discuss how we can further streamline referrals, improve patient transitions, or provide additional support, we are here for you.
Let’s continue working together to make every patient’s experience one of dignity, peace, and compassionate care.
Connor, S. R., Teno, J., Spence, C., & Smith, N. (2020). Family perceptions of quality in hospice care: Findings from the National Hospice and Palliative Care Organization Family Evaluation of Hospice Care Survey. Journal of Pain and Symptom Management, 60(4), 719-725.
Dixon, J., King, D., Matosevic, T., Clark, M., & Knapp, M. (2015). Equity in the provision of palliative care in the UK: Review of evidence. Journal of Palliative Medicine, 18(1), 3-15.
Teno, J. M., Gozalo, P. L., Bynum, J. P., Leland, N. E., Miller, S. C., Morden, N. E., & Mor, V. (2016). Change in end-of-life care for Medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA, 309(5), 470-477.
Hospice care is built upon a foundation of compassion, dignity, and support – not only for the patient but also for their family and loved ones. While medical teams provide expert pain and symptom management, hospice volunteers bring an irreplaceable level of companionship, emotional support, and non-medical assistance that enhances quality of life in the final stages.
Despite their essential role, many healthcare professionals are unaware of just how much volunteers contribute to hospice care. This is where we stand apart – our volunteers are at the heart of everything we do.

Our dedicated hospice volunteers extend their care in profound ways that benefit both patients and their loved ones, including:
Research shows that volunteer involvement in hospice care has a measurable impact:

Many hospice providers mention volunteers in passing, but few truly leverage them as a core part of their care model. Our hospice program prioritizes volunteer integration in ways that make a tangible difference, ensuring:
Choosing the right hospice provider for your patients means selecting a team that goes beyond symptom management – it means selecting a provider that values the whole-person approach, including the emotional and psychosocial support volunteers bring.
Refer your patients to a hospice that treats volunteers as an essential part of the care team. Contact us today to learn more about how our hospice services stand apart.
Candy, B., France, R., Low, J., Sampson, E. L., & Vickerstaff, V. (2020). Does involving volunteers in the provision of palliative and end-of-life care improve patient and family well-being? A systematic review of quantitative and qualitative evidence. Journal of Pain and Symptom Management, 60(2), 302-312.
Connor, S. R., Pyenson, B., Fitch, K., Spence, C., & Iwasaki, K. (2019). Comparing hospice and nonhospice patient survival among patients who die within a three-year window. Journal of Pain and Symptom Management, 40(5), 704-710.
Ghesquiere, A., Hauser, J., & Schulz, R. (2021). Family caregiver burden and hospice use: The impact of volunteer support. The Gerontologist, 61(1), 108-117.
National Hospice and Palliative Care Organization (NHPCO). (2023). NHPCO facts and figures: Hospice care in America. https://www.nhpco.org/hospice_statistics
When a patient enters hospice, care does not end at the moment of passing – it extends far beyond, reaching the hearts of those left behind. Our bereavement support team provides critical emotional and psychological assistance to families, caregivers, and loved ones, ensuring they are not alone in their grief. This is a vital component of hospice care that is often underappreciated yet profoundly impactful.
Our bereavement specialists are trained professionals who provide ongoing support to those who have lost a loved one. Their work includes:

Hospice bereavement support is not just compassionate – it is essential. Studies have shown that unresolved grief can contribute to mental health challenges such as depression, anxiety, and even physical illness (Shear et al., 2011). Additionally, well-structured bereavement programs have been linked to improved family coping mechanisms, lower incidences of prolonged grief disorder, and reduced hospitalizations for bereaved individuals due to stress-related conditions (Guldin et al., 2012).
Referring a patient to hospice means providing comprehensive support that extends beyond physical care – it ensures that their loved ones are supported long after they are gone. Our bereavement services are a cornerstone of this commitment, giving families the guidance and tools to process their grief in a healthy, supported manner.
We invite you to partner with us to ensure your patients and their loved ones receive the full spectrum of care they deserve. Contact us today to learn more about how our hospice team can provide unparalleled bereavement support, making a lasting difference for families in need.
Christakis, N. A., & Iwashyna, T. J. (2003). The health impact of health care on families: A matched cohort study of hospice use by decedents and mortality outcomes in surviving, widowed spouses. Social Science & Medicine, 57(3), 465-475.
Guldin, M. B., Vedsted, P., Zachariae, R., Olesen, F., & Jensen, A. B. (2012). Complicated grief and need for professional support in family caregivers of cancer patients in palliative care: A longitudinal cohort study. Supportive Care in Cancer, 20(8), 1679-1685.
NHPCO. (2021). Facts and figures: Hospice care in America. National Hospice and Palliative Care Organization. Retrieved from https://www.nhpco.org
Shear, M. K., Frank, E., Houck, P. R., & Reynolds, C. F. (2011). Treatment of complicated grief: A randomized controlled trial. JAMA, 293(21), 2601-2608.
Wright, A. A., Zhang, B., Ray, A., Mack, J. W., Trice, E., Balboni, T., & Prigerson, H. G. (2008). Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA, 300(14), 1665-1673.
Vietnam Veterans have a distinct set of needs at the end of life, and we are honored to provide care that respects their service and sacrifices. Our compassionate team is skilled in addressing physical, emotional, and spiritual challenges, including the impact of post-traumatic stress disorder (PTSD).

1. Recognize the Need: Refer patients who could benefit from pain management, emotional support, and spiritual care.
2. Contact Us: Call us to learn how we can collaborate.
3. Submit the Referral: Once we communicate, we will coordinate the next steps seamlessly.
Let’s work together to give Vietnam Veterans the respect and care they deserve during their final chapter.
Every day, you rise to the challenge of bringing hope and resources to those who need it most. Whether it’s guiding a family through difficult decisions, connecting patients to life-changing support, or simply offering a listening ear – your work goes far beyond the ordinary. You are the steady hand when life feels overwhelming, the compassionate voice in moments of uncertainty, and the driving force behind the well-being of so many. Your dedication shapes the lives of countless individuals in ways that can never be measured. We see your resilience. We admire your selflessness. And we celebrate the impact you make in skilled nursing facilities, specialty practices, hospitals, and beyond.
We are so grateful to partner with you in making a difference. You inspire us to approach our work with the same passion and commitment to helping those in need.
From our entire team, thank you for being extraordinary.

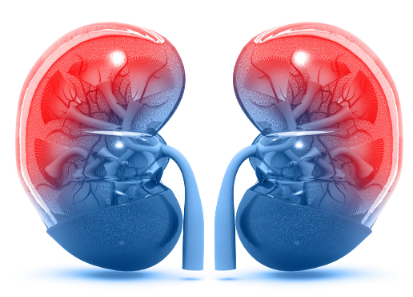
Kidney disease ranks among the leading causes of death in the United States, with over 37 million Americans living with chronic kidney disease (CKD) and millions more at risk (National Institute of Diabetes and Digestive and Kidney Diseases [NIDDK], 2023). For patients who progress to end-stage renal disease (ESRD), the challenges of managing symptoms, maintaining quality of life, and navigating care options can feel overwhelming.
When curative treatments are no longer effective or desired, hospice care offers a specialized approach to providing comfort, dignity, and peace during the final stages of life.
Hospice care is a holistic, interdisciplinary service designed to meet the physical, emotional, and spiritual needs of patients and their families. For those with ESRD, hospice care provides:

Patients with ESRD are eligible for hospice care if they meet specific criteria, such as:
If you have a patient or loved one facing end-stage kidney disease, hospice care can provide comfort and support during this challenging time. Our compassionate team is here to answer your questions, guide you through the process, and help ensure the best possible quality of life.
Contact us today to learn more about how hospice care can make a difference for those living with kidney-related diseases.
Meier, D. E., Morrison, R. S., & Aldridge, M. D. (2023). Timely hospice care and improved outcomes
for patients with end-stage kidney disease. Journal of Palliative Medicine, 26(3), 250-260.
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2023). Kidney disease
statistics for the United States. Retrieved from https://www.niddk.nih.gov

As a hospice care provider, we understand the complexities and challenges of managing end-stage heart conditions. These advanced stages of heart disease can significantly impact the quality of life, making it essential to consider supportive care options that prioritize comfort and dignity.
According to the Centers for Medicare & Medicaid Services (CMS), patients with heart disease qualify for hospice care if their life expectancy is six months or less, as certified by a physician (CMS, 2022).
If you or a loved one is living with an advanced heart condition, consider how hospice care can help maintain dignity, comfort, and peace during this challenging time. Our team is here to provide expert care and guidance every step of the way.
Contact us today to learn more about hospice services for patients with end-stage heart conditions. Let us help you make the most of every moment. Contact us for details.